Services
Our Mission
We have noticed plan design shortcomings and a lack of claim coordination leads to increased employer liability. Our team takes the time to get to know our client’s workforce to provide innovative solutions offering practical coverage.
60 Million
Americans lack access to affordable, quality healthcare
1 in 2
Adults admit they have delayed or avoided medical care due to finances

7 out of 10
Americans have less than $1,000 in savings
1 in 3
Workers report their health worsened as a result of care
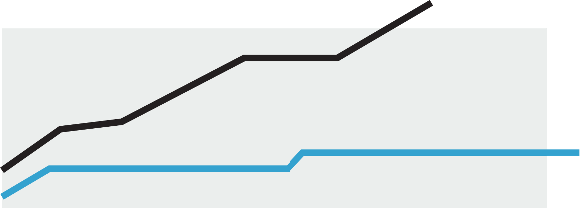
284%
Insurance premiums have grown by 284% while workers wages have fallen behind inflation
We Fix Your Healthcare™
BenefitsDNA provides employers, plan sponsors, and Taft-Hartley funds with Healthcare and benefits advisory services. We broker insurance plans on behalf of our clients, striving for fee-based arrangements to align our incentives with our clients’ success. Collectively, our team investigates and understands the US Healthcare marketplace educating plan sponsors on their options with the ultimate goal of decreasing costs and/or enhancing coverage. Day-to-day, BenefitsDNA advocates for clients and their members ensuring they have the resources to use their benefits as they are intended without suffering undue costs or lower-quality care. Our goal every day is to get one step closer to an improved healthcare system where those who need it can afford it and will live better lives because of it.
Putting it together

Our Clients
BenefitsDNA advises large group plan sponsors across all industries. We understand that each plan has a unique DNA with differing needs, budgets, demographics, and benefits. Our clients are in fully insured, level-funded, captive and self-funded arrangements depending on their size, risk appetite, and other pertinent factors. There is no one-size-fits-all in healthcare and every BenefitsDNA client receives individualized attention.
Compliance Audit
Implications of the Consolidated Appropriations Act (CAA)
- Gag Clause Prohibition Compliance Attestation (GCPCA)
- CMS Prescription Drug Reporting Submissions (RxDC)
- Direct, Indirect, Non-Monetary Compensation Disclosure of Covered Service Providers
- MHPAEA Attestation
Ongoing Compliance Monitoring
- Plan Document, SPD, Section 125, Wrap Documents
- 5500 Filings
- 1095/1094 Reporting
- PCORI Fee
- And More
Covered Service Providers
- Insurance Broker, Consultant
- Insurance Carriers
- Benefits Administration Technology
- Pharmacy Benefits Managers
- Medical Management
- Employee Assistance Programs
- Point Solutions
- Third Party Administrators
Our Process
BenefitsDNA’s goal is to provide innovative, impactful solutions for plan sponsors with respect to their healthcare and health insurance costs. It would be pompous to think we could do that without getting to know the people that drive our clients’ businesses to understand their specific healthcare needs. We engage active decision-makers to comprehend your past, present, and what you’d like the future to hold. This information in conjunction with the data we request grants BenefitsDNA the ability to paint that future as well as educate on the necessary steps to achieve that vision. We succeed when our clients succeed.
Actuarial Reporting & Analysis
Actuaries on staff provide our clients with an array of services
Budgeting,
Forecasting,
IBNR Reports
ASC 965 Valuations
Insurance Capitation Studies
Part D Attestations
MHPAEA Analysis
SBC Due Diligence
COBRA Rate Development
Provider Network Analysis
Plan Design Analysis
